LIVER CANCER
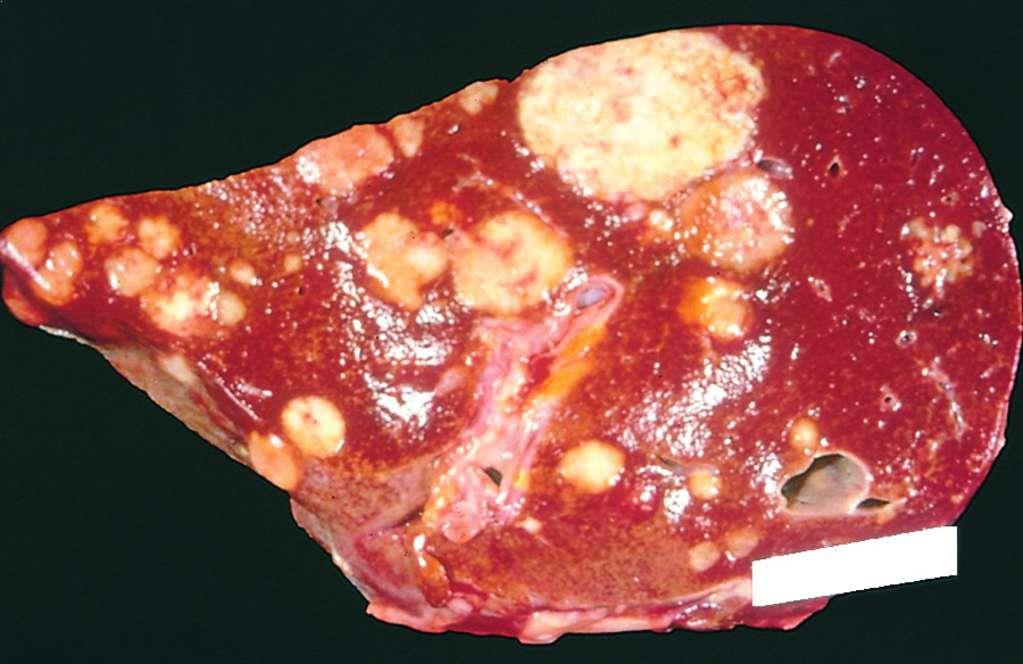
Liver cancer is cancer that begins in the cells of your liver. The most common type of liver cancer is hepatocellular carcinoma(HCC), which begins in the main type of liver cell (hepatocyte). Other types of liver cancer, such as intrahepatic cholangiocarcinoma (IHCC) and hepatoblastoma, are much less common.
Not all cancers that affect the liver are considered liver cancer. Cancer that begins in another area of the body — such as the colon, lung or breast — and then spreads to the liver is called metastatic cancer. Cancer that spreads to the liver is more common than cancer that begins in the liver cells.
Most people don't have signs and symptoms in the early stages of primary liver cancer. When signs and symptoms do appear, they may include:
- Losing weight without trying
- Loss of appetite
- Upper abdominal pain
- Nausea and vomiting
- General weakness and fatigue
- Abdominal swelling
- Yellow discoloration of your skin and the whites of your eyes (jaundice)
- White, chalky stools
Causes of Liver Cancer
Cirrhosis can have a number of different causes including:
- Chronic infection with HBV or HCV
- Certain inherited liver diseases - Hemochromatosis and Wilson's disease.
- Primary biliary cirrhosis
- Diabetes. People with this blood sugar disorder have a greater risk of liver cancer than those who don't have diabetes.
- Nonalcoholic fatty liver disease. An accumulation of fat in the liver increases the risk of liver cancer.
- Excessive alcohol consumption. Consuming more than a moderate amount of alcohol daily over many years can lead to irreversible liver damage and increase your risk of liver cancer.
You may be able to significantly reduce your chances of developing liver cancer by:
- Avoiding or cutting down on alcohol
- Eating healthily
- Exercising regularly
- Taking steps to reduce your risk of becoming infected with hepatitis B and C
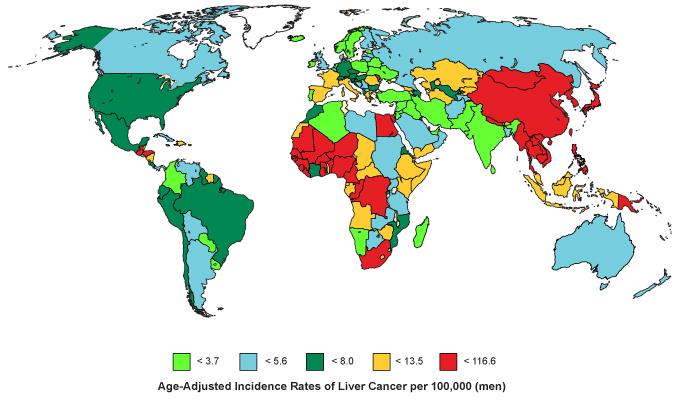
Liver cancer screening
For the general population, screening for liver cancer hasn't been proved to reduce the risk of dying of liver cancer, so it isn't generally recommended. The American Association for the Study of Liver Diseases recommends liver cancer screening for those thought to have a high risk, including people who have:
- Hepatitis B and one or more of the following apply: are Asian or African, have liver cirrhosis, or have a family history of liver cancer
- Hepatitis C infection and liver cirrhosis
- Liver cirrhosis from other causes, such as an autoimmune disease, excessive alcohol use, nonalcoholic fatty liver disease and inherited hemochromatosis.
- Primary biliary cirrhosis
Diagnosing Liver Cancer
Tests and procedures used to diagnose liver cancer include:
- Blood tests: Liver function tests, Tumor markers
- Imaging tests: Ultrasound, Computerized tomography (CT) scan and Magnetic resonance imaging (MRI)
- Removing a sample of liver tissue for testing: Your doctor may recommend removing a piece of liver tissue (Liver biopsy) for laboratory testing in order to make a definitive diagnosis of liver cancer.
Treating Liver Cancer
Treatment for liver cancer depends on the stage the condition is at. If diagnosed early, it may be possible to remove the cancer completely.
Treatment options in the early stages of liver cancer include:
- Surgical resection – surgery to remove a section of liver
- Liver transplant where the damaged cancerous liver is replaced with a new healthy liver. Liver transplant surgery is only an option for a small percentage of people with early-stage liver cancer.
- Localized treatments: Microwave ablation/ Radiofrequency ablation/ Injecting alcohol into tumor cells
However, only a small proportion of liver cancers are diagnosed at a stage where these treatments are suitable. Most people are diagnosed when the cancer has spread too far to be removed or completely destroyed.
In these cases, treatments such as chemotherapy are used to slow down the spread of the cancer and relieve symptoms such as pain and discomfort.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.